A 35 year-old woman presented to the ED with complaints of right sided facial numbness, right arm weakness, and right leg weakness that began one hour prior to arrival. She had a headache that started 24 hours ago. She reports a past medical history of two CVAs but is taking no medications and cannot explain why she had a stroke at such a young age and in the absence of any risk factors. On exam, she has no objective findings (no facial droop, dysarthria, etc). Her strength, while slightly weaker in the right arm and leg, remains 5/5 throughout. She receives a generous score of 3 on the NIH scale.
Stat CT head is unremarkable. Recognizing that this is likely a complicated migraine but that she will be a difficult disposition given her reported history, I asked for a tele-neurology consultation. Our hospital doesn’t have the benefit of an in-house neurologist so if someone is a tPA candidate or there is concern for acute stroke, we ask a remote neurologist to evaluate the patient via a computer screen. I had no doubt that the hospitalist would want this done as this patient was likely headed towards admission.
About twenty minutes later I was shocked when the nurse exited the room and told me the neurologist is recommending that we push tPA. When I asked how he came to that decision, the nurse shook his head and said ‘the patient told him she wanted it’. A few minutes later I had the official consultation in hand from the neurologist confirming that his recommendation was to administer tPA. Perplexed, I asked to speak to him and our conversation went something like this:
Me: “Are you crazy?!”
Him: “A low NIH is not a contraindication for tPA.”
Me: “I never said it was! But why would you want to give this to her?”
Him: “She has weakness. There are no contraindications. Why not give it to her?“
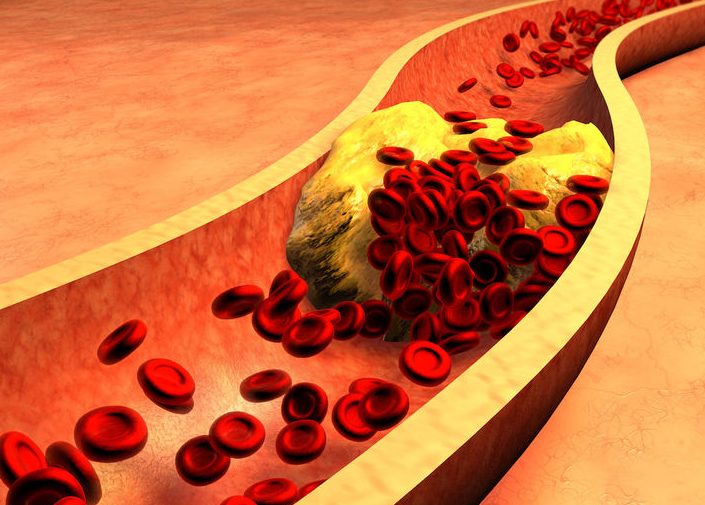
After a few minutes of going in circles, I kindly thanked him and hung up the phone. I looked again at his note. He checked off that he discussed all risks/benefits with the patient. I went back into the room and found the patient laughing and using her cell phone. Her headache had improved but she still felt ‘a little weak’ in her right arm and leg. I asked her if he had discussed the risks of tPA with her and she said ‘no, but I heard it busts up clots so let’s try it, right?’
Taking a deep breath I pulled up a chair and explained the potential for an intracranial bleed. I told her that my recommendation differed from his, that he was the expert, but we would ultimately do what she wanted. She simply shrugged and said ‘well, you’ve seen me. If you don’t think I need it, then let’s skip it.’
I don’t want to enter into a debate about the merits of tPA. This is an ongoing issue for discussion. I recognize that in the right situation tPA has benefits, but I also recognize that the studies were flawed and feel that it is over-used by neurologists. When it’s your license on the line, rely on your clinical judgement and hopefully take advantage of a good relationship with your patient to have an open and frank discussion.