Your first patient of the day hobbles in to a room. He’s an odd-looking elderly man. Before you can ask what’s wrong, he shouts, “My toe is killing me! I think it’s the gout acting up!” Pleased that he has revealed his diagnosis with literally no effort on your part, you start to smile. Your happiness is short-lived however, as he asks, “So, are you gonna check my uric acid level or not?” You wake up in a cold sweat and realize you have very strange dreams. Try as you might, you just can’t shake the image of the strange man with the inflamed toe.
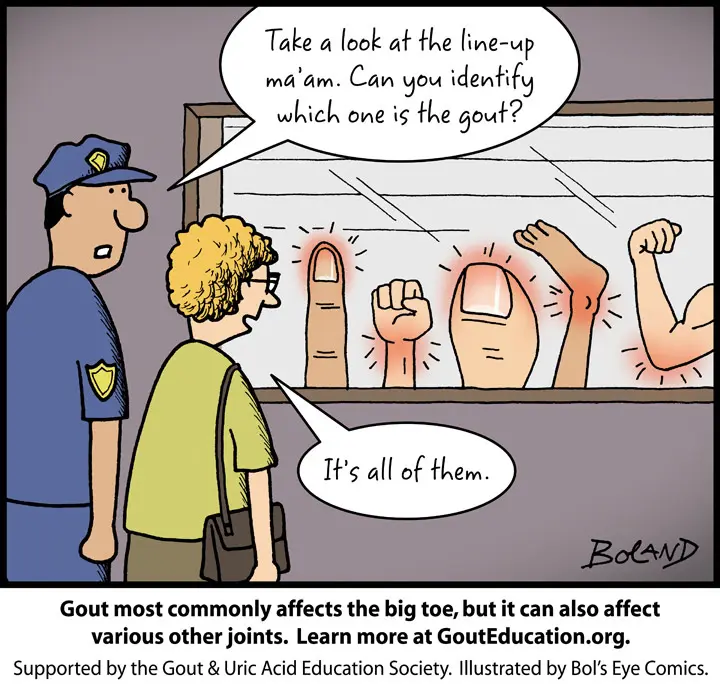
How does gout present?
An acute attack of gout is characterized by the sudden onset of severe pain and swelling. Gout flares are typically monoarticular, and the most commonly involved joint is the first MTP (big toe). The ankle and knee are the next most commonly affected. Gout can occur in almost any other joint but these are the most commonly affected areas.
Any risk factors?
Local trauma, alcohol binges, overeating or fasting, weight changes, and use of diuretics may precipitate an acute attack.
Are labs helpful?
White blood cell count, ESR, and CRP are typically elevated during an acute flare. Still, these are nonspecific labs and do not rule in or rule out the diagnosis.
The most important reason to check these labs is to rule out other causes of acute monoarticular pain, ie septic arthritis.
What about Uric Acid levels?
During an acute flare, serum uric acid level may be high, normal, or low. High uric acid levels are helpful in the clinical diagnosis of gout in symptomatic patients, but hyperuricemia alone does not definitively confirm the diagnosis.
In patients suspected of gout based on clinical features, elevated serum urate level can support the diagnosis but is neither diagnostic nor required to establish the diagnosis. The most accurate time for assessing serum urate level to establish a baseline value is two weeks or more after a gout flare completely subsides. In other words, checking a level shortly after the flare has begun (which is often when the patient will present to an urgent care or ER) carries little utility in patients with an established history of gout.
How the pros do it:
The true way to diagnose gout is by identifying the presence of uric acid crystals in synovial fluid or from a tophaceous deposit. In the setting of an acute gout attack, aspiration of joint fluid (by using a needle to draw fluid out of the swollen joint) and examination of the fluid under polarized light can yield the definitive diagnostic finding of needle shaped negatively-birefringent uric acid crystals. Intracellular crystals within a neutrophil are characteristic during an acute attack (good to know for boards, not so relevant otherwise).
As the clincal features of acute gout and a septic joint can be very similar, arthrocentesis is important to rule out infection by sending the joint fluid for culture in these circumstances. Importantly, gout and infection can co-exist in the same joint (they are not mutually exclusive) and consideration should be made for sending joint fluid for culture even in a patient with an established history of gout if they are at risk for infection.

Treatment of an acute gout flare
First-line treatment is NSAIDs, colchicine, or systemic glucocorticoids. The length of the treatments should be at least 7 to 10 days to prevent rebound flare-ups.
NSAIDs
NSAIDs are most effective when initiated within 48 hours of the onset of gout symptoms. Indomethacin (50 mg three times daily) or naproxen (500 mg twice daily), are good choices. There is no convincing data that favors one NSAID over another. Typically NSAID treatment for gout flare lasts for seven days.
Contraindications for the use of NSAIDs include active duodenal or gastric ulcer, cardiovascular disease (uncontrolled hypertension or heart failure), and chronic kidney disease.
Oral Glucocorticoids
Glucocorticoids are recommended in gout patients with contraindications to NSAIDs and/or colchicine. These agents are also drugs of choice for patients with renal insufficiency. The initial dose for gout flare is 50 mg of prednisone once daily for 7 to 10 days. This has been proven to be at least comparable to NSAID efficacy.
Colchicine
Colchicine has been shown to reduce pain by over 50% in a randomized control trial at 24 hours compared to a placebo. The total dose of colchicine should not exceed 1.8 mg on day 1 (either 1.2 mg for the first dose followed by 0.6 mg an hour later [US Food and Drug Administration (FDA) approved dose] or 0.6 mg three times on the first day. On subsequent days, colchicine should be taken once or twice daily until the resolution of a gout flare.
A reduced dose of colchicine may be required for patients with diminished hepatic or renal function or potential drug interactions. The most common adverse effects of colchicine are abdominal cramping and diarrhea.
TLDR:
Checking a uric acid level may carry some utility in a patient who has never been diagnosed with gout, as elevated levels can support the diagnosis
There’s little value in checking a uric acid level on every patient with an established history of gout who presents with an acute flare
An acute flare can present with normal OR high levels of uric acid
NSAIDs, colchicine, +/- steroids is the optimal treatment