A 16-year old baseball player presents with left testicle pain. He was sliding into a base about 12 hours ago when the discomfort began, and it has intermittently continued throughout the night. He looks pretty uncomfortable:

Here’s what UptoDate has to say about ‘acute scrotal pain’:
“The initial evaluation of acute scrotal pain includes a directed history and physical examination.”
There’s an old saying that you can ‘ace the exam but fail the patient’. Taking a directed history and physical are important, before even entering the room, you should order a testicular ultrasound. There are few absolutes in medicine, but I would venture that ANYONE with acute onset scrotal pain should absolutely have a testicular ultrasound.
That being said, there are some important historical questions to ask: timing of the onset of pain, presence of fever or discharge, etc.
Your immediate differential diagnosis for acute onset scrotal pain boils down to three things:
1. Torsion
2. Epididymitis
3. Fourniere’s gangrene
Fourniere’s is easy: if the patient has perineal tenderness/induration/fluctuance, fever, presence of immunosuppression – consider this one. It’s a clinical diagnosis and warrants immediate surgical consultation before any results are even back.
The best way to distinguish torsion from epididmytis is with a Doppler ultrasound.
If you’re taking a boards exam, check a cremasteric reflex. Lightly stroke the inner part of the thigh to make the cremaster muscle contract and pull up the ipsilateral testis. If the cremasteric reflex is negative (the testis does not pull up when the ipsilateral thigh is stroked), it suggests testicular torsion.
If the cremasteric reflex is positive (the testis pulls up when the ipsilateral thigh is stroked), acute epididymo-orchitis or orchitis is the likely diagnosis.
The epididymis is a ‘spongy’ tube-like structure which is best palpated along the posterior aspect of each testicle. Even if there is isolated epididymal tenderness and the patient has a history suggestive of STD and the patient’s a urologist and says “I have epididymitis” – he or she (hey, you never know nowadays) still warrants a testicular ultrasound.
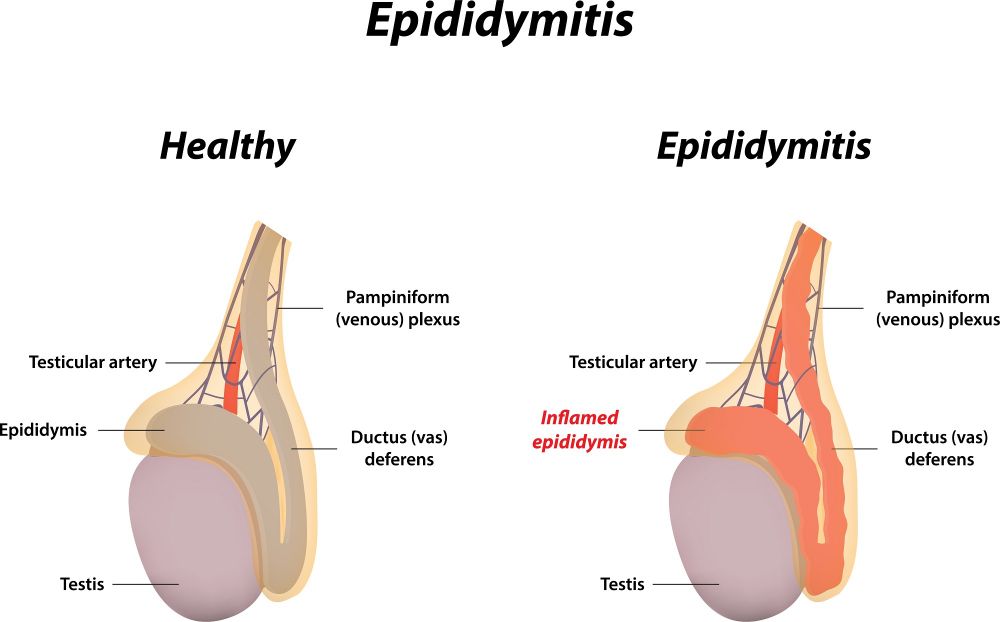
In men under the age of 35, Gonorrhea / Chlamydia are the most common causes. In men over the age of 35, E. coli and Pseudomonas are more common (often in association with BPH and obstructive uropathy). You will need to tailor antibiotics accordingly.
What is torsion?
The lower pole of the testicle should be fixated to the tunica vaginalis. Otherwise it may torse (twist) on the spermatic cord, leading to ischemia. It can be spontaneous or following some minor innocuous trauma.
Treatment is detorsion and fixation of both testicles as inadequate fixation is typically a bilateral defect.
What is the “golden period”?
You’ve probably heard ‘time is heart’ to describe MIs or ‘time is brain’ to describe strokes. Well, time is also testicle. It’s important to ask when the patient’s pain started and traditional teaching is that extended periods of ischemia (pain > 12 hours duration) makes surgery almost futile.
A September 2017 article called this into question. Over 2000 cases of testicular torsion were reviewed and salvage rates were as follows:
0 to 6 hours : 97.2%
7 to 12 hours : 79.3%
13 to 18 hours : 61.3%
19 to 24 hours : 42.5%
25 to 48 hours : 24.4%
> 48 hours : 7.4%
(Source: A Systematic Review of Testicle Survival Time After a Torsion Event. Pediatr Emerg Care. 2017 Sep 25.)
Put another way, there was a nearly 25% salvage rate for torsion that presented 24 hours later! Patients with torsion should have immediate urology consultation. If you really suspect this, make the call before an ultrasound is even performed.
What about the appendix testis?
Torsion of the appendix testis is most common in children, ages 7-14. Pain is more gradual in onset. You may see the ‘blue dot’ sign which indicates infarction and necrosis of the appendix testis. Doppler would show good flow to both testicles. Management is ice and NSAIDs. If pain is persistent, surgery may be necessary.

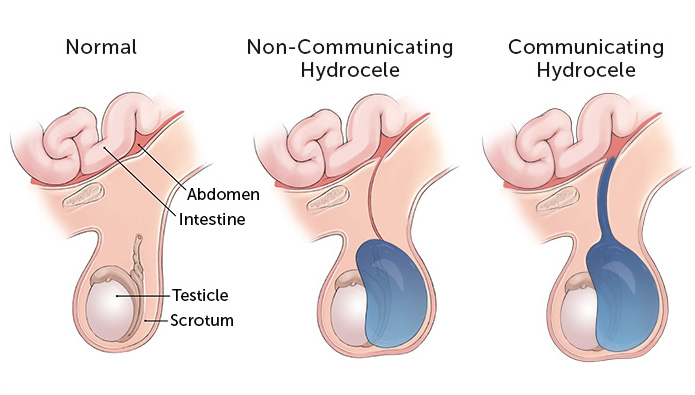
What about hydroceles?
Hydroceles are typically without complication and will not affect fertility. But it might be a clue to an underlying malignancy. It can also be found after an infection like epididymitis. When discovered in children, they usually go away by the age of 2. If it does not go away or gets fairly large, it should be removed.