By far the most common denominator in a successful malpractice suit is ‘missed diagnosis’. Studies have shown that up to 80% of malpractice lawsuits are for this reason.
This case, based on an actual lawsuit with some details changed to protect those involved, began with a chief complaint of ‘fever’. The patient’s temperature was documented as 101F. On review of systems, he complained of fatigue, cough, nausea, diarrhea, and joint pain. Labs revealed bacteria in his urine and the fever was chalked up to a UTI. The patient was discharged home with antibiotics for a urinary tract infection.
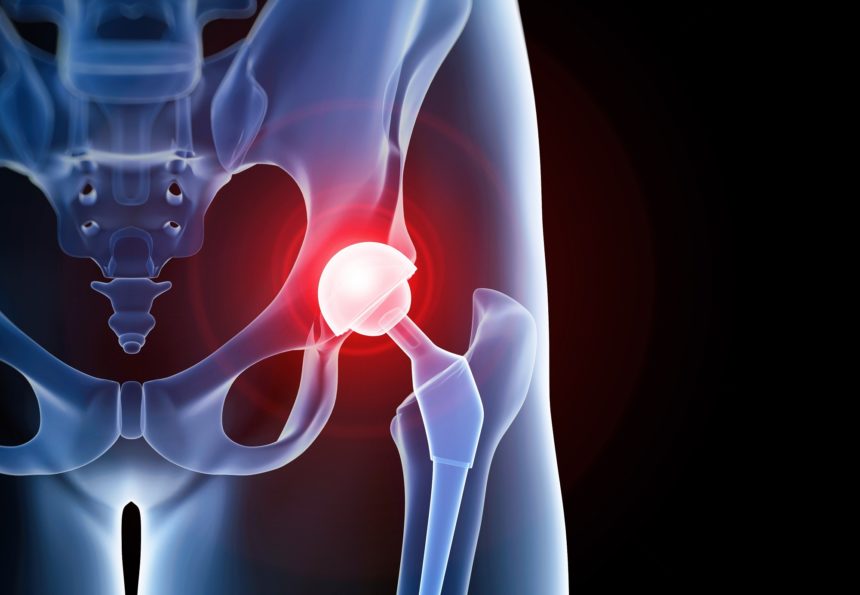
One key part of the history which was overlooked: the patient had undergone a total hip arthroplasty roughly 20 years prior to his presentation. Why would a THA that was done two decades ago be relevant?
Strangely enough, blood cultures were sent off prior to discharge. When they began to grow Gram + bacteria, later identified as MRSA, the patient returned to the hospital. This time, he was admitted. It took a few days for the providers to put the pieces together and by the time a septic prosthetic joint was diagnosed, it was too late. The patient went into multi-system organ failure and died.
The defendant Emergency Physician’s attorney claimed that the patient would have died from MRSA septicemia even if the correct diagnosis had been made on the initial visit. An expert witness testified on his behalf that chronic prosthetic joint infections are so rare that the doctor could not have reasonably been expected to make the diagnosis. The case was dismissed.
Sounds like a win for the Emergency Room doctor right? The case was dismissed! Wrong. There are no winners in a medical malpractice case. There are only losers who lost a little less than the other losers. If we can educate ourselves and learn from the experiences of others, then maybe we can hope to prosper from this unfortunate case.
Peri-prosthetic joint infection (PJI) is one of the most devastating complications following total joint arthroplasty. Early PJI develops within 3 months of surgery and manifests with acute joint pain, warmth, and erythema.
However, PJI may develop tens of years later [as it did in this case] when a person has any type of infection (bacteremia, UTI, etc) that spreads to the hip. Suspect PJI when there is hip pain, erythema, or some complaint related to the hip in a patient with fever.
Take-home point: beware atraumatic joint pain. While it may be easy to chalk it up to some type of arthralgia, good documentation of the physical exam and your rationale is essential. Document a good differential to show that you considered high-risk diagnoses: it’s much easier to defend your decision-making if you show that you considered them and ruled them out, even if they are missed, than it is if it appears as if you never even considered them.
One final note: in this case, ordering the cultures may have inadvertently been the one thing that could have saved the patient. In reality, ordering cultures on a discharged patient is something you should almost never do. Strongly reconsider ordering any test whose results you will not personally be following up on.