The Case
A 30 year old woman gave birth to a baby after nearly 20 hours in labor. Three days later she started having fever, chills, and abdominal pain. At this point, there really isn’t any need to provide additional information as the ‘diagnosis until proven otherwise’ is pretty much clinched. If you don’t consider and rule out endometritis, then you’re asking for trouble.
The ED was staffed solely by an NP – there was an ED physician available for telephone consultation if needed, but he/she was not in house. Temperature was 101.8. Labs showed a leukocytosis and thrombocytopenia.
Urinalysis was suggestive of infection (there were white blood cells, but also squamous epithelial cells and a lack of any bacteria). The patient was discharged home with a diagnosis of UTI. There was no phone call or conversation with an OB. She returned later that day unresponsive. After resuscitation and regaining a pulse, she was taken to the OR where it was discovered that she had endometritis. The cause of death is listed as ‘severe sepsis’. Defense argued that she died of necrotizing fasciitis and that any delay in treatment was moot as the outcome would not have been any different. The treating surgeon disagreed.
The outcome
Family was awarded over $20 million in damages, making it the largest medical malpractice case in state history.
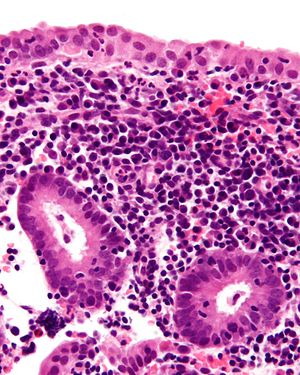
Endometritis
Early postpartum abdominal pain and fever is endometritis until proven otherwise. Other key features include uterine tenderness, purulent lochia, and chills. Patients will have signs of sepsis. Remember that the white blood cell count is often physiologically elevated postpartum. But presence of a left shift and rising neutrophil count suggests an infectious process. Look at the whole clinical picture: an isolated mildly elevated white blood cell count may be acceptable. In the setting of fever, tachycardia, and abdominal pain, an elevated WBC count is concerning.
The diagnosis of postpartum endometritis is clinical. Treatment is broad-spectrum antibiotics; clindamycin + gentamicin is most commonly used.
Most cases of endometritis develop within the first week after delivery, but it may present up to six weeks later. Delayed presentation is more common following vaginal delivery.
Boards stuff
Here’s the question you may be asked: what is the most common organism isolated from patients with endometritis?
Postpartum endometritis is typically a polymicrobial infection involving a mixture of two to three aerobes and anaerobes from the genital tract. Some sources claim Group B Strep is the most common organism in the first 24 hours and mixed aerobes/anaerobes are isolated at 3-7 days postpartum.
Sexually transmitted infections (Neisseria gonorrhoeae and Chlamydia trachomatis) are rare causes of postpartum endometritis, but much more common in cases of endometritis unrelated to pregnancy.
The number one risk factor for endometritis is cesarean delivery (especially when performed after the onset of labor). Bacterial vaginosis is an important pathogen in the setting of cesarean delivery.
Take-home points
Know the sepsis criteria!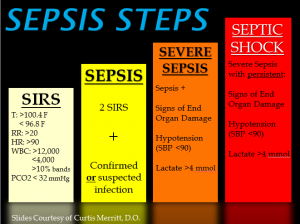
Thrombocytopenia is also an indicator of severe sepsis
Get your consultants involved! They are there to support you and the worst thing they will do is raise a fuss over being called. Patient who have undergone recent procedures almost always deserve a call to that physician. One of the biggest mistakes we can make is not using the resources that are available to us.
This patient was diagnosed with a ‘UTI’ despite having no bacteria in the urine. She met sepsis criteria, so if you think she has a UTI then the proper diagnosis is more likely ‘pyelonephritis’. Pyelonephritis in such a recent postpartum patient would still warrant OB consultation and likely admission. Be very wary of explaining a high fever and sepsis away as an uncomplicated urinary tract infection.