An infant presented to the ER with vomiting. Mother noted the child had less energy than usual and vomited twice in the last 24 hours; twice more while in the ED. He was afebrile, and per the ED note, this is what was free-texted under the physical exam:
“appears ill, lethargic, eyes mildly sunken”
The child received Zofran, passed a PO challenge, and was discharged home.
He returned less than 24 hours later with intractable vomiting. The child was ill appearing, had a weak cry, and was dehydrated.
Labs and an LP were unremarkable, antibiotics were initiated, and he was admitted to the pediatrics service. Just before he could leave the department, something in my gut told me we were missing something. CT scan of his brain is shown below:

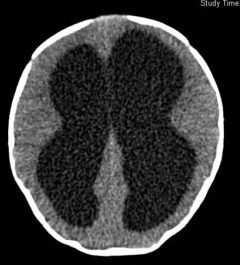
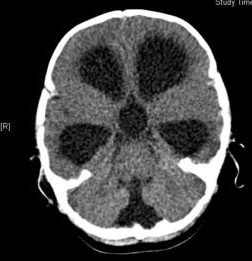
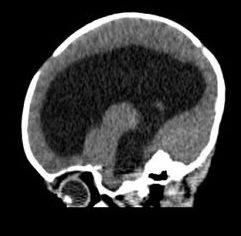
The official read is: “severe communicating hydrocephalus without hemorrhage”.
There’s a lot to learn from this case. It’s unfair and nearly impossible to question the care that was delivered on the first visit. I can’t say I would have done anything differently.
Be very careful about the language you choose to include in a patient’s chart. If your care is questioned, the chart is the only thing that can be used to exonerate you. Avoid potentially dangerous phrases/buzzwords (like the word ‘lethargic’) and if you must use them, spend extra time in the medical decision-making section explaining how you addressed those findings.
If a patient bounces back with a legitimate acute complaint, I almost always double the workup and very seldom send the patient home. Performing cultures and a lumbar puncture would have been adequate and it would be hard to fault a physician for not ordering a CT scan on an infant with vomiting.




